Issue of the Week: Disease


Two years later, coronavirus evolution still surprises experts, National Geographic, 3.11.2022
Two years ago tomorrow, the World Health Organization declared Covid 19 a global pandemic.
The rest is history–6 million deaths later in the official count (certainly much higher in reality, much less millions more dying from impacts creating a further lack of basic needs), with countless millions more suffering from ongoing disease and symptoms, other medical issues, economic disaster, hunger–and scars of various kinds affecting billions, virtually everyone.
Except that it’s not history yet, as much as it seems like it may be going in that direction, and as much as we want it to be.
Although cases and deaths in the US have been dropping significantly and probably will continue to for now, there were still over a thousand deaths per day today. Two years ago when the pandemic was offically declared, and the US was on the verge of locking down, there were 38.
With everything else going on, (as we pointed out previously, war may now be replacing the pandemic as the predominant apocalyptic danger), and with our overhwelming desire to push aside the two years of unique global trauma of the pandemic, this two year mark is more of an unspoken melancholia than would be normal.
Which as always when pushing aside reality, could be our undoing.
Today, hauntingly, China, where it all began, locked down the city of Jilin, where an outbreak of a sub-strain of the Omicron variant has been found. The number of covid cases in China doubled today from the day before, near to a two year-high. The cases are small in number by global standards, but the percentages are another wake up call.
National Geographic has posted an article on where we’ve been and why it’s not over (dated tomorrow as we write in our time zone), and another a few days ago on the dangers of avoidance in the aftermath demonstrated by the 1918 pandemic.
Both must reads, with many related links. Here they are:
“Two years later, coronavirus evolution still surprises experts. Here’s why.”
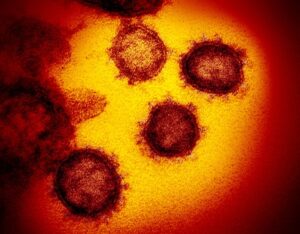
Scientists and physicians continue to be amazed by how quickly the virus evolves, what it does to the human body, and how it moves through species.
PUBLISHED MARCH 11, 2022
Raul Andino knows his pathogens. For more than 30 years the University of California, San Francisco researcher has studied RNA viruses, a group that includes the virus that causes COVID-19. And yet he never imagined he’d witness a pandemic of this scale in his lifetime.“The magnitude of it and the implications of it are still hard to comprehend,” Andino says.Although experts in his field suspected a pandemic would occur, “it’s hard to know when,” he says. “It’s similar to an earthquake—you know the earthquake will happen, but normally you don’t think about it.”On March 11, 2020—exactly two years ago—the World Health Organization declared COVID-19 to be a pandemic. The disease has since infected nearly 500 million people in almost 200 countries and killed more than six million people worldwide, and it’s not over yet.Along the way, this coronavirus has presented scientists with a bevy of surprises: Many experts are still amazed by how quickly the virus evolves, what it does to the human body, and how it moves in and out of other species.The original SARS-CoV-2 virus rapidly evolved into a string of variants that have hindered a return to pre-pandemic normalcy. Even with the virus’s genetic blueprint in hand and the ability to decode the genomes of new variants within hours, virologists and healthcare professionals struggle to predict how its mutations will alter the virus’s transmissibility and severity.Millions of people are grappling with symptoms that linger for weeks to several months after they’d been diagnosed with an infection. Scientists are racing to understand the biology of this new and perplexing syndromecalled long COVID.
Two years in, there’s still a lot we don’t know about SARS-CoV-2, says David Wohl, an infectious disease specialist at the University of North Carolina. Here’s what scientists have uncovered so far—and the mysteries that continue to tantalize and frustrate coronavirus experts.
Worst-case scenario
Experts had been warning of some kind of looming pandemic for decades. As humans expand settlements into wild areas, they raise the odds of a new pathogen jumping from an animal to a person, giving rise to a deadly zoonotic disease. A study published in Nature showed that emerging infectious diseases originating in wildlife had increased significantly between 1940 and 2004.
But most experts were worried about influenza viruses and would not necessarily have expected a coronavirus to cause such havoc.
That changed with the 2002-04 Severe Acute Respiratory Syndrome (SARS) outbreak, which infected more than 8,000 people in 29 countries and left 774 dead. Then the 2012 Middle East Respiratory Syndrome (MERS) outbreak infected more than 2,000 people in 37 countries; that virus has so far killed nearly 900.
Still, people weren’t paying as much attention to coronaviruses compared to the “really bad guys” like influenza, HIV, dengue viruses, Andino says.
Then SARS-CoV-2 arrived with a bang. It was spreading faster than previous coronaviruses, and one reason, scientists suspect, is its ability to move efficiently from one cell to the next. SARS-CoV-2 is also harder to contain because it causes so many asymptomatic cases, people who can then unknowingly spread the virus. “In a way, SARS-CoV-2 has found a way in which it can [rapidly] spread and also cause disease,” Andino says. “It’s the worst-case scenario playing out.”
March of the variants
Adding to the oddities, the SARS-CoV-2 virus acquired genetic mutations much more rapidly than expected.
Coronaviruses usually mutate at lower rates than other RNA viruses, like influenza and HIV. Both SARS-CoV and SARS-CoV-2 accumulate approximately two mutations each month; half to one sixth the rate seen in influenza viruses. That’s because coronaviruses have proofreading proteins that correct errors introduced into the virus’ genetic material as it replicates.
“That’s why we thought [SARS-CoV-2] would not evolve very fast,” says Ravindra Gupta, a clinical microbiologist at the University of Cambridge.
But the virus quickly proved Gupta and his colleagues wrong. The emergence of Alpha—the first variant of concern identified in the United Kingdom in November 2020—stunned scientists. It had 23 mutations that set it apart from the original SARS-CoV-2 strain, eight of which were in the spike protein, which is essential for anchoring to human cells and infecting them.
“It became clear that the virus could make these [surprising] evolutionary leaps,” says Stephen Goldstein, an evolutionary virologist at the University of Utah. With this set of mutations, Alpha was 50 percent more transmissible than the original virus.
The next version, Beta, was first identified in South Africa and was reported as a variant of concern just a month later. It carried eight mutations on the viral spike, some of which helped the virus escape the body’s immune defenses. And when the Gamma variant emerged in January 2021, it had 21 mutations, 10 of which were in the spike protein. Some of these mutations made Gamma highly transmissible and enabled it to reinfect patients who previously had COVID-19.
“It’s surprising to see these variants make pretty significant leaps in transmissibility,” Goldstein says. “I just don’t think we’ve observed a virus do that before, but of course, we have not actually observed any pandemics previously with the amount of genetic sequencing capacity we have now.”
Then came Delta, one of the most dangerous and contagious variants. It was first identified in India and designated a variant of concern in May 2021. By late 2021 this variant dominated in almost every country. Its unique constellation of mutations—13 overall and seven in the spike—made Delta twice as infectious as the original SARS-CoV-2 strain, led to longer lasting infections, and produced 1,000 times more virus in the bodies of infected people.
“It [SARS-CoV-2]’s ability to come up with new solutions and ways to adapt and spread with such ease—it’s incredibly surprising,” Andino says.
However, Omicron, which is two to four times more contagious than Delta, rapidly replaced that variant in many parts of the world. First identified in November 2021, it carries an unusually high number of mutations—more than 50 overall and at least 30 in the spike—some of which help it evade antibodies better than all the earlier virus versions.
“These huge jumps [in mutations] make the pandemic far less predictable,” says Francois Balloux, a computational biologist at the University College London Genetics Institute in the United Kingdom.
Chronic infections
One of the most compelling explanations for the huge leaps in the number of mutations is that that the SARS-CoV-2 virus was able to evolve for long periods of time in the bodies of immunocompromised people.
During the past year, scientists have identified cancer patients and people with advanced HIV disease who were unable to get rid of their COVID-19 infection for months to nearly a year. Their suppressed immune systems enabled the virus to persist, replicate, and mutate for months.
Gupta identified one such mutation (also seen in the Alpha variant) in a sample from a cancer patient who remained infected for 101 days. In an advanced HIV patient in South Africa who was infected for six months, scientists recorded a multitude of mutations that helped the virus escape the body’s immune defenses.
“That the virus is changing its biology this quickly in its evolutionary history is a huge find,” Gupta says. Other viruses like influenza and norovirus also undergo mutation in immunocompromised individuals, but “it is very rare,” Gupta says, and they “infect a narrow range of cells.”
By contrast, SARS-CoV-2 has proven capable of infecting many different areas of the body—creating yet more baffling effects for scientists to untangle.
Not just a respiratory virus
Early in the pandemic medical professionals noticed that the virus wasn’t just causing pneumonia-like illness. Some hospitalized patients also presented heart damage, blood clots, neurologic complications, and kidneyand liver defects. Mounting studies within the first few months suggested one reason why.
SARS-CoV-2 uses proteins called ACE2 receptors on the surface of human cells to infect them. But because ACE2 is present in many organs and tissues, the virus was infecting more parts of the body than just the respiratory tract. There were also a few reports of the virus, or parts of it, in blood vessel cells, kidney cells, and small quantities in brain cells.
“I’ve studied a lot of pandemics, and in almost all of them, you look at the brain, you’ll find the virus there,” says Avindra Nath, a neuroimmunologist at the National Institutes of Health. For instance, brain autopsy tissues from 41 hospitalized and dead COVID-19 patients revealed low levels of the virus. But there were also clear signs of damage, including dead neurons and mangled blood vessels.
“That’s the biggest surprise,” Nath says.
It’s likely that the virus triggers the body’s immune system to go into a hyperactive mode called a cytokine storm, which causes inflammation and injury to different organs and tissues. An abnormal immune response can persist even after infection, resulting in lingering symptoms including chronic fatigue, heart palpitations, and brain fog.
“But there are virus reservoirs that can cause chronic inflammation,” says Sonia Villapol, a neuroscientist at the Houston Methodist Research Institute. A recent study that’s not yet been peer-reviewed showed that SARS-CoV-2 genetic material could persist for up to 230 days in the body and brains of COVID-19 patients, even in those who harbored only mild or asymptomatic infections.
Susan Levine is an infectious-disease doctor in New York who specializes in the treatment and diagnosis of chronic fatigue syndrome, which has parallels with long COVID. She now sees 200 patients every week, compared to 60 in pre-pandemic times. Unlike CFS, long COVID “hits you like a ton of bricks,” Levine says. “It’s like a tornado inside your body where you’re going from working 60 hours a week down to being in the bed all day within a week of getting the infection. The action is so compressed.”
Animal reservoirs of SARS-CoV-2
Scientists are now concerned about the persistence of SARS-CoV-2 outside human populations and its potential to spread to other animals and jump back into humans, possibly extending the pandemic.
In April 2020 tigers and lions at New York’s Bronx Zoo tested positive for COVID-19, sparking interest in finding other animals that might be susceptible. Soon after a study identified mammals including certain primates, deer, whales, and dolphins to be among the most vulnerable to COVID-19 given the similarity between their ACE2 receptors and the counterpart in human cells.
Another study used a machine learning approach to assess the abilities of 5,400 mammal species to transmit SARS-CoV-2; it found that several animals most at risk of spreading COVID-19 were those living alongside people, such as livestock and even pets.
So far SARS-CoV-2 has infected pet cats, dogs, and ferrets, ravaged mink farms, and spread to tigers, hyenas, and other animals in zoos. What’s more, SARS-COV-2 has successfully jumped from humans to captive minks and back into mink farmers. And a person in Canada was potentially infected with COVID-19 when the virus jumped from a white-tailed deer.
“The concern is if it continues to evolve in deer to a point where deer become more and more immune to it, their preexisting antibodies from their reinfection could also further drive viral evolution,” says Samira Mubareka at Canada’s Sunnybrook Health Sciences Centre. Also, “the virus may be circulating in other animals out there.”
Still, the spread of SARS-CoV-2 among humans continues to be a bigger concern for scientists, as they learn more about the virus and its presence and impact in both humans and animals.
“We still don’t know what the future holds,” Wohl says. “We’ll be two years plus of history and track record, and even then with that knowledge, it’s still hard to predict what will happen.”
. . .
“The lessons learned from 1918 flu fatigue, according to historians”
More than a century ago, exhausted Americans just wanted to forget about two years of lockdowns and mask mandates—but experts warn against repeating history.
PUBLISHED MARCH 4, 2022
Two decades after surviving an influenza pandemic that devastated the United States, Katherine Anne Porter recounted her experiences in one of the best-known accounts of the period—the 1939 novella Pale Horse, Pale Rider.
In her story, Porter describes how many young people felt as though their lives were threatened by the dual strike of a deadly virus and World War I. Miranda, the main character, recovers from influenza, but sinks into depression as she attempts to rejoin society. The novella ends on a note of optimism, however, where Miranda dreams of a world with no war and no more plague, and she’d have time for “everything.”
Historians say it’s unclear when the 1918 flu actually did end—and that’s partly because Americans were as tired of the flu as they are now after two years of COVID-19. Although cases continued to spike in 1920 and beyond, much of the historical record of the pandemic is from its first two years. Porter’s novella is one of the few written accounts of its enduring trauma and formal efforts to document the disease ultimately failed because Americans in the early 20th century simply wanted to forget the flu.
Similarly, two years into the COVID-19 pandemic, fatigue has grown—alongside arguments about when to loosen public health measures like mask and vaccine mandates. But historian Nancy Bristow, who wrote about the novella in her book American Pandemic: The Lost Worlds of the 1918 Influenza Epidemic, says that while going back to a pre-pandemic normal may be appealing, history shows it could have harmful implications both for this pandemic—and the next one.
“That drive to not have to do what we’ve been doing carries with it a great potential to forget,” she says. “The ways in which Americans continue to think that these kinds of things won’t happen to us, that kind of American exceptionalism, you can only do that if you are a nation that is very, very capable of forgetting moments of its past.”
Fatigue sets in over public health measures
Flu historians like Bristow point out that these two pandemics can’t quite be neatly compared. The world was dramatically different in the early 20th century—war was widespread, there were no influenza vaccines, and the U.S. didn’t have as robust a health care infrastructure to care for those who fell ill then. The virus also targeted younger populations and the pandemic response wasn’t politicized nearly as much as it has been now.
But there are some similarities. During the early waves of the 1918 flu, there was a patchwork of public health responses from states and local authorities—and the outcomes of their various approaches to flattening the curve was clear. Cities like New York that implemented public health measures early had low death rates. Meanwhile, cities like Philadelphia that waited to implement health measures—and those like San Francisco that relaxed their measures too early—had higher death rates. (Here’s how U.S. cities flattened the curve during the 1918 flu pandemic.)
Then, like now, there was also confusion about when to change or relax measures, says Thomas Ewing, a historian based at Virginia Tech. In Denver, Colorado, officials rescinded their mask mandate in November 1918 when the first outbreak of influenza had tapered down, but then a second wave hit the city, causing many to question if the mandate should be reinstated.
“In both pandemics, there’s been a lot of confusion, there’s been uncertainty, there’s been resistance, there’s been conflicting, contradictory recommendations,” Ewing says.